
ASCUS, LSIL or CIN1?
A ASCUS, LSIL or CIN1 is a mild abnormality or in other, more scientific or medical words, a pre-cancerous lesion, with great emphasis on "pre-”cancerous. It is not cancer and the likelihood of it becoming cancer is very low! That's why many people use the following comparison: It is a type of common cold, but not pneumonia that requires hospital treatment.
ASCUS stands for: Atypical Squamous Cells of Undetermined Significance
LSIL stands for Low grade Squamous Intraepithelial Lesion Both terms are used when a cervical smear was the basis of the diagnosis.
CIN1 stands for Cervical Intraepithelial Neoplasia grade 1 and is used if a biopsy was taken.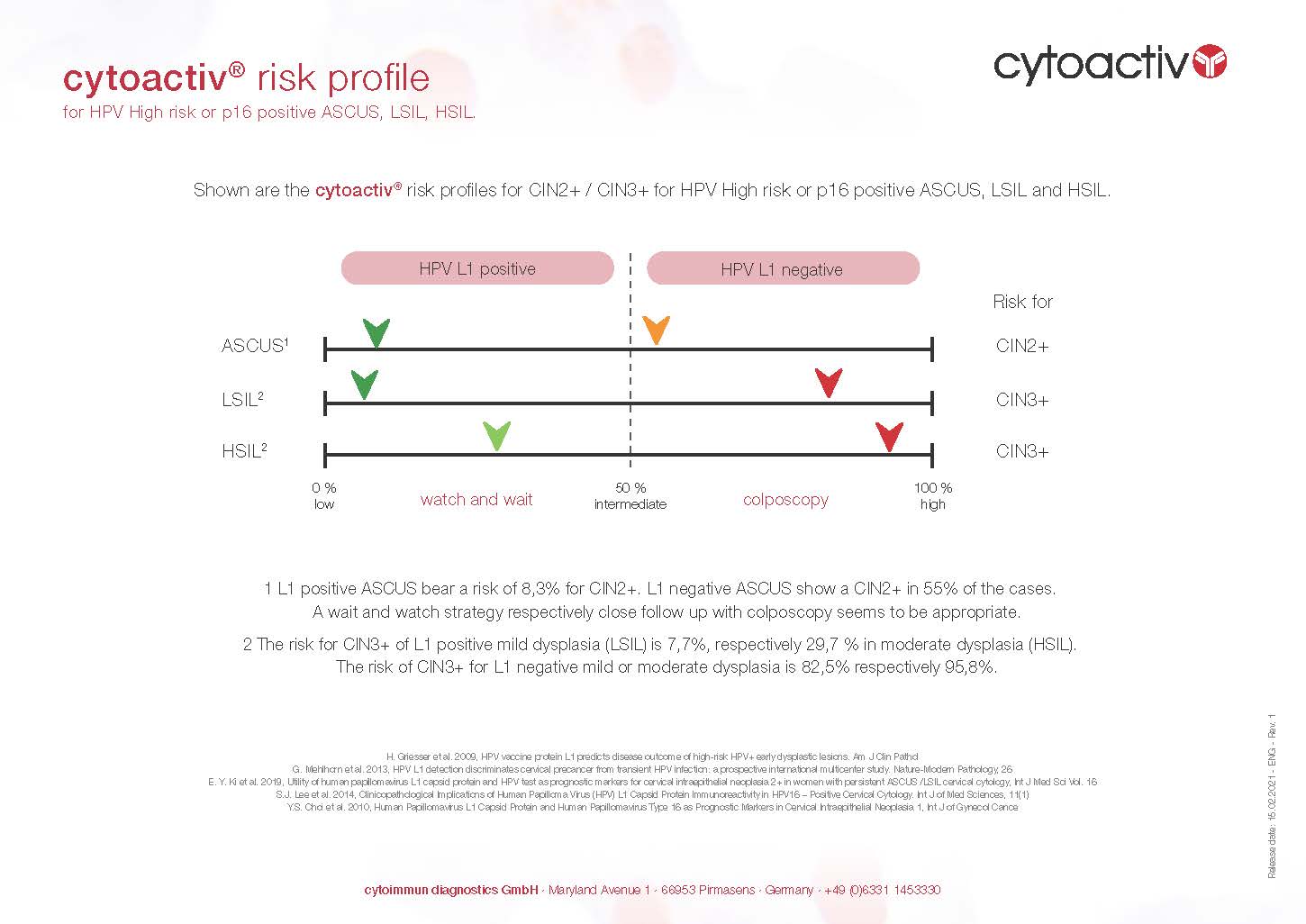


Development
In most women, this pre-cancerous stage heals on its own within 1 – 2 years without anything having to be done. In most cases the immune system is fighting successfully against disease. Only in very few women (approx. 5 percent) does the precancerous stage progress slowly and eventually become cancer, typically about 10 years later.
What to do?
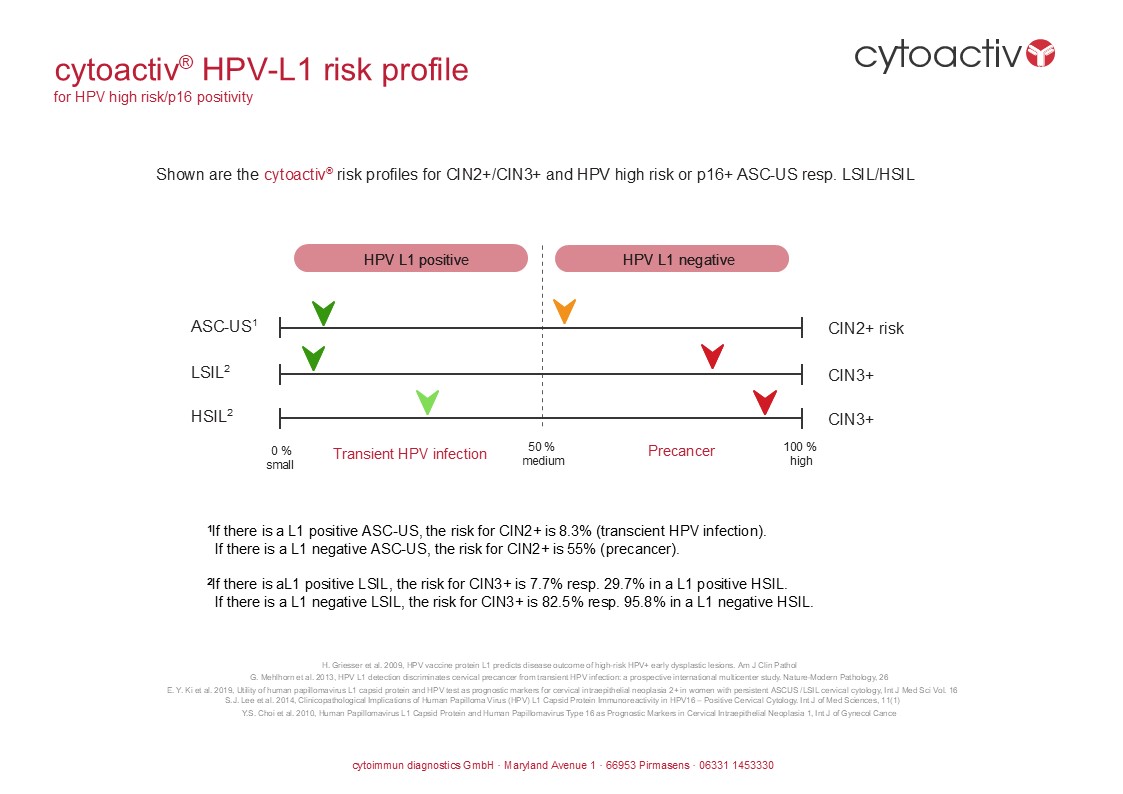
By detecting the capsid protein L1, every woman can find out whether her ASCUS/LSIL/CIN1 will disappear on its own or not: simply, quickly and reliably! Scientifically confirmed by many studies.
L1 - what is that?
The L1 capsid protein is a so-called prognostic protein, i.e. it predicts the further course of the cell changes with a high degree of probability.
How do I prove L1?
L1 is detected on a smear test or a biopsy. The gynecologist can request the L1 test from the laboratory by referral and the health insurance company will cover the costs, in most countries worldwide.
I have the L1 - what now?
Great! Now you can wait and drink tea. Your immune system is defending itself against the altered cells. Promote your immune system by living healthy; reduce smoking or drinking alcohol if relevant in your life style. However, as a kind of watchful waiting, you should still visit your gynecologist every 3-6 months for a smear test.
I don't have an L1 - what now?
Too bad. Your immune system has not recognized the threat and is not doing anything about it. Talk to your gynecologist about what measures should be taken now. A retesting should be considered to see if 3-6 month later the L1 situation has changed.
When does it become cancer?
On average, it takes between 5 and 10 years for a ASCUS/LSIL/CIN1 to develop into cancer. So plenty of time to take the right steps – and no acute danger that should tempt you to make hasty decisions that you may regret one day.
When to have a cone?
Conization should be considered, as the immune system is not activated by the missing L1. The earlier, the better, as this prevents the altered cells from spreading further.
If a smear is abnormal, an HPV test is carried out to determine whether it was caused by human papillomavirus. The types are also determined; often the high-risk types 16 and 18, but there are others. Unfortunately, determining the HPV type does not indicate whether the altered cells will regress on their own or not.
Various vaccines against HPV are available, but they only work optimally if they are administered before the first sexual intercourse. You can find more information here: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer

(https://en.wikipedia.org/wiki/Bethesda_system)

If not only a cell smear is taken with a brush, but also a tissue sample (biopsy), which reveals abnormal findings, this is classified as CIN (for Cervical Intraepithelial Neoplasia). These are also precursors of cervical cancer.
A distinction is made between three stages:
CIN I describes a mild cell change in the cervix, similar to LSIL.
CIN II describes a moderate cell change, similar to HSIL.
CIN III describes a severe cell change. In this case, there is a high probability of a transition to cervical cancer. For this reason, conization is often recommended for CIN III.
Who pays the costs for the L1 analysis?
Cytoactiv – HPV L1 detection
Scientific publications (commented)
E. Y. Ki et al., 2019
Utility of human papillomavirus L1 capsid protein and HPV test as prognostic markers for cervical intraepithelial neoplasia 2+ in women with persistent ASCUS / LSIL cervical cytology.
International Journal of Medical Sciences, Vol. 16, p. 1096
Absence of HPV L1 capsid expression and presence of HPV type 16 or 18 infection are reliable predictors of progression to CIN2+. Only 4.1% of Cytoactiv-positive LSIL and 13.8% of Cytoactiv-positive ASCUS progressed. 89% of progressive cases were HPV16/18 positive. Only 1.5% of non-HPV16/18, L1-positive cases progressed.
F. Carozzi et al., 2018
Molecular Cytology Applications on Gynecological Cytology. In: Schmitt F. (eds) Molecular Applications in Cytology.
Springer
Chapter 8.3.1 “Biomarkers of the Productive Phase of the HPV-Induced Carcinogenesis” provides an overview of Cytoactiv HPV L1 detection.
Y.-J. Choi et al., 2018
E2/E6 ratio and L1 immunoreactivity as biomarkers to determine HPV16-positive high-grade squamous intraepithelial lesions (CIN2 and 3) and cervical squamous cell carcinoma.
Journal of Gynecologic Oncology
Validation of HPV L1 capsid protein expression combined with decreased HPV E2/E6 ratio as predictive markers of ≥CIN2 lesions. Using 226 ThinPrep slides, Cytoactiv was shown to be effective in combination with HPV integration markers. Combined AUC was 0.87.
G. Mehlhorn et al., 2014
HPV16-L1-specific Antibody Response Is Associated with Clinical Remission of High-risk HPV-positive Early Dysplastic Lesions.
Anticancer Research 34: 5127–5132
Detection of HPV16-L1-specific antibodies strongly correlates with clinical remission. The risk of progression to CIN3 in L1 antigen and HPV16-L1 antibody double-positive women is extremely low (approx. 6%).
S.-J. Lee et al., 2014
Clinicopathological Implications of HPV L1 Capsid Protein Immunoreactivity in HPV16-Positive Cervical Cytology.
International Journal of Medical Sciences, 11(1):80–86
HPV L1 expression is low in advanced dysplasia. Absence of L1 in HPV16-positive ASCUS and LSIL is strongly associated with high-grade histopathology (≥CIN3).
G. Mehlhorn et al., 2013
HPV L1 detection discriminates cervical precancer from transient HPV infection: a prospective international multicenter study.
Modern Pathology, 26: 967–974
Prospective multicenter study (n=908) confirmed that only ~20% of L1-positive cases progressed to CIN3, whereas 84% of L1-negative cases progressed. Cytoactiv reliably distinguishes transient from progressive HPV infections.
S. W. Byun et al., 2013
Immunostaining of p16INK4a/Ki-67 and L1 Capsid Protein on Liquid-based Cytology Specimens from ASC-H and LSIL-H Cases.
International Journal of Medical Sciences
Combined analysis of p16INK4a, Ki-67 and L1 capsid protein improves prediction of high-risk precursor or invasive cervical lesions.
R. Hilfrich, 2013
HPV L1 Detection as a Prognostic Marker for Management of HPV High Risk Positive Abnormal Pap Smears.
InTech – Human Papillomavirus
Comprehensive summary of scientific data supporting Cytoactiv as a prognostic marker in abnormal Pap smear management.
I. Norman et al., 2013
High-risk HPV L1 capsid protein as a marker of cervical intraepithelial neoplasia in HR-HPV-positive women with minor abnormalities.
Oncology Reports 30
Loss of L1 expression predicts CIN2+. L1-positive ASCUS/LSIL lesions have low malignant potential and support a “wait and see” strategy.
Ch. A. Brown et al., 2012
Role of Protein Biomarkers in the Detection of High-Grade Disease in Cervical Cancer Screening Programs.
Journal of Oncology, Volume 2012
Review of protein biomarkers including Ki-67, p16INK4a, BD ProEx C and Cytoactiv HPV L1.
L. Benerini-Gatta et al., 2011
Diagnostic Implications of L1, p16, and Ki-67 Proteins in Low-grade Cervical Intraepithelial Neoplasia.
International Journal of Gynecological Pathology
Malignant transformation correlated with L1– / p16+ cases (100% of CIN2/3 and SCC). Approximately 23% of CIN1 cases showed malignant transformation.
G. Böhmer, Th. Weyerstahl, 2011
Management of abnormal results of the cervix uteri during cervical cancer screening.
Thieme Gynaecology up2date
Review of current management recommendations; Cytoactiv clearly distinguished as a prognostic marker.
S. J. Lee et al., 2011
Correlation between HPV L1 immunocytochemistry and behavior of low-grade cervical cytology.
Journal of Obstetrics and Gynaecology Research
Positive predictive value of HPV L1-positive cases for non-progression was 91.7%.
M. T. Galgano et al., 2010
Using Biomarkers as Objective Standards in the Diagnosis of Cervical Biopsies.
American Journal of Surgical Pathology
Cytoactiv showed superior specificity (96.7%) and highest reproducibility compared to p16 and Ki-67.
Y. S. Choi et al., 2010
HPV L1 Capsid Protein and HPV16 as Prognostic Markers in CIN1.
International Journal of Gynecological Cancer
HPV L1 protein expression is closely related to spontaneous regression in CIN1.
H. Griesser et al., 2009
HPV vaccine protein L1 predicts disease outcome of HR-HPV+ early dysplastic lesions.
American Journal of Clinical Pathology
Progression occurred in only 20% of L1-positive cases versus 97% of L1-negative cases.
Th. Scheidemantel et al., 2008
Expression pattern of HPV L1 capsid protein in PAP tests.
Abstract, American Society of Cytopathology
None of the Cytoactiv-positive patients progressed to cervical cancer.
G. Negri et al., 2008
p16 and HPV immunohistochemistry in low-grade dysplastic lesions.
American Journal of Surgical Pathology
Confirms prognostic value of Cytoactiv and benefit of combination with p16 and HPV testing.
R. Hilfrich, J. Hariri, 2008
Prognostic relevance of HPV L1 detection combined with p16.
Analytical and Quantitative Cytology and Histology
Progression in 83.9% of L1-negative cases versus 27.5% of L1-positive cases; Cytoactiv specificity 100%.
D. Rauber et al., 2008
Prognostic significance of HPV L1 detection in mild to moderate dysplasia.
European Journal of Obstetrics & Gynecology and Reproductive Biology
Progression rate of L1-positive cases was only 12.3%.
H. Griesser et al., 2004
Correlation of HPV L1 detection with regression of HR-HPV positive dysplasia.
Analytical and Quantitative Cytology and Histology
First Cytoactiv publication demonstrating strong prognostic value of HPV L1 detection.
Imprint
Information according to § 5 TMG:
Cytoimmun Diagnostics GmbH
Maryland Avenue 1
66953 Pirmasens
Represented by:
Managing Director Albert Hirtz
Contact:
|
Phone: |
+49 6331 145333-0 |
|
Fax: |
+49 6331 145333-99 |
|
E-Mail: |
info@cytoimmun.de |
Register entry:
Entry in the commercial register.
Register court: Register court Zweibrücken
Register number: HRB 23724
Sales tax ID:
Value added tax identification number in accordance with §27 a Value Added Tax Act:
DE814317161
Supervisory authority:
State Office for Social Affairs, Youth and Care, Mainz
Privacy policy
We are very delighted that you have shown interest in our enterprise. Data protection is of a particularly high priority for the management of the Cytoimmun Diagnostics GmbH. It is generally possible to use the Cytoimmun Diagnostics GmbH website without providing any personal data. However, if a person concerned wishes to make use of special services of our company via our website, it may be necessary to process personal data. If the processing of personal data is necessary and there is no legal basis for such processing, we generally obtain the consent of the data subject.
The processing of personal data, such as the name, address, e-mail address, or telephone number of a data subject shall always be in line with the General Data Protection Regulation (GDPR), and in accordance with the country-specific data protection regulations applicable to the Cytoimmun Diagnostics GmbH. By means of this data protection declaration, our company would like to inform the public about the type, scope and purpose of the personal data we collect, use and process. Furthermore, data subjects are informed of their rights by means of this privacy policy.
As the controller, Cytoimmun Diagnostics GmbH has implemented numerous technical and organizational measures to ensure the most complete protection of personal data processed through this website. Nevertheless, Internet-based data transmissions can generally have security gaps, so absolute protection cannot be guaranteed. For this reason, every data subject is free to transmit personal data to us by alternative means, for example by telephone.
1. definitions
The data protection declaration of Cytoimmun Diagnostics GmbH is based on the terms used by the European legislator for the adoption of the General Data Protection Regulation (GDPR). Our privacy policy should be easy to read and understand for the public as well as for our customers and business partners. To ensure this, we would like to explain the terminology used in advance.
We use the following terms, among others, in this privacy policy
(a) personal data
Personal data is any information relating to an identified or identifiable natural person (hereinafter "data subject"). An identifiable natural person is one who can be identified, directly or indirectly, in particular by reference to an identifier such as a name, an identification number, location data, an online identifier or to one or more factors specific to the physical, physiological, genetic, mental, economic, cultural or social identity of that natural person.
b) Data subject
Data subject is any identified or identifiable natural person whose personal data is processed by the controller responsible for the processing.
c) Processing
Processing is any operation or set of operations which is performed on personal data or on sets of personal data, whether or not by automated means, such as collection, recording, organization, structuring, storage, adaptation or alteration, retrieval, consultation, use, disclosure by transmission, dissemination or otherwise making available, alignment or combination, restriction, erasure or destruction.
d) Restriction of processing
Restriction of processing is the marking of stored personal data with the aim of restricting its future processing.
e) Profiling
Profiling means any form of automated processing of personal data consisting of the use of personal data to evaluate certain personal aspects relating to a natural person, in particular to analyze or predict aspects concerning that natural person's performance at work, economic situation, health, personal preferences, interests, reliability, behavior, location or movements.
f) Pseudonymization
Pseudonymization is the processing of personal data in such a manner that the personal data can no longer be attributed to a specific data subject without the use of additional information, provided that such additional information is kept separately and is subject to technical and organizational measures to ensure that the personal data are not attributed to an identified or identifiable natural person.
g) Controller or controller responsible for the processing
The controller or controller responsible for the processing is the natural or legal person, public authority, agency or other body which, alone or jointly with others, determines the purposes and means of the processing of personal data. Where the purposes and means of such processing are determined by Union or Member State law, the controller or the specific criteria for its nomination may be provided for by Union or Member State law.
h) Processor
Processor is a natural or legal person, public authority, agency or other body which processes personal data on behalf of the controller.
i) Recipient
Recipient is a natural or legal person, public authority, agency or another body, to which the personal data are disclosed, whether a third party or not. However, public authorities which may receive personal data in the framework of a particular inquiry in accordance with Union or Member State law shall not be regarded as recipients.
j) third party
A third party is a natural or legal person, public authority, agency or body other than the data subject, controller, processor and persons who, under the direct authority of the controller or processor, are authorized to process personal data.
k) Consent
Consent is any freely given, specific, informed and unambiguous indication of the data subject's wishes by which he or she, by a statement or by a clear affirmative action, signifies agreement to the processing of personal data relating to him or her.
2. name and address of the controller
The controller within the meaning of the General Data Protection Regulation, other data protection laws applicable in the Member States of the European Union and other provisions of a data protection nature is
Cytoimmun Diagnostics GmbH
Maryland Avenue 1
66953 Pirmasens
Pirmasens, Germany
Phone: 063311453330
E-mail: hallo@pap-3d.de
Website: www.pap-3d.de
3. cookies
The Internet pages of Cytoimmun Diagnostics GmbH use cookies. Cookies are text files that are placed and stored on a computer system via an Internet browser.
Numerous websites and servers use cookies. Many cookies contain a so-called cookie ID. A cookie ID is a unique identifier of the cookie. It consists of a string of characters that can be used to assign websites and servers to the specific internet browser in which the cookie was stored. This enables the websites and servers visited to distinguish the individual browser of the data subject from other Internet browsers that contain other cookies. A specific Internet browser can be recognized and identified via the unique cookie ID.
Through the use of cookies, the Cytoimmun Diagnostics GmbH can provide the users of this website with more user-friendly services that would not be possible without the cookie setting.
By means of a cookie, the information and offers on our website can be optimized for the benefit of the user. As already mentioned, cookies enable us to recognize the users of our website. The purpose of this recognition is to make it easier for users to use our website. For example, the user of a website that uses cookies does not have to re-enter their access data each time they visit the website because this is taken over by the website and the cookie stored on the user's computer system. Another example is the cookie for a shopping basket in an online store. The online store remembers the items that a customer has placed in the virtual shopping cart via a cookie.
The data subject can prevent the setting of cookies by our website at any time by means of a corresponding setting of the Internet browser used and thus permanently object to the setting of cookies. Furthermore, cookies that have already been set can be deleted at any time via an Internet browser or other software programs. This is possible in all common Internet browsers. If the person concerned deactivates the setting of cookies in the Internet browser used, not all functions of our website may be fully usable.
4. collection of general data and information
The website of Cytoimmun Diagnostics GmbH collects a series of general data and information each time the website is accessed by a data subject or an automated system. This general data and information is stored in the server log files. The (1) browser types and versions used, (2) the operating system used by the accessing system, (3) the website from which an accessing system accesses our website (so-called referrer), (4) the sub-websites which are accessed via an accessing system on our website can be recorded, (5) the date and time of access to the website, (6) an internet protocol address (IP address), (7) the internet service provider of the accessing system and (8) other similar data and information used for security purposes in the event of attacks on our information technology systems.
When using these general data and information, the Cytoimmun Diagnostics GmbH does not draw any conclusions about the data subject. Rather, this information is needed to (1) deliver the content of our website correctly, (2) optimize the content of our website as well as its advertisement, (3) ensure the long-term viability of our information technology systems and website technology, and (4) provide law enforcement authorities with the information necessary for criminal prosecution in case of a cyber-attack. Therefore, the Cytoimmun Diagnostics GmbH analyzes anonymously collected data and information statistically, with the aim of increasing the data protection and data security of our enterprise, and to ensure an optimal level of protection for the personal data we process. The anonymous data of the server log files are stored separately from all personal data provided by a data subject.
5. contact possibility via the website
The website of Cytoimmun Diagnostics GmbH contains information that enables a quick electronic contact to our enterprise, as well as direct communication with us, which also includes a general address of the so-called electronic mail (e-mail address). If a data subject contacts the data controller by e-mail or via a contact form, the personal data transmitted by the data subject is automatically stored. Such personal data transmitted on a voluntary basis by a data subject to the controller are stored for the purposes of processing or contacting the data subject. This personal data is not passed on to third parties.
6 Routine erasure and blocking of personal data
The controller shall process and store the personal data of the data subject only for the period necessary to achieve the purpose of storage, or as far as this is granted by the European legislator or other legislators in laws or regulations to which the controller is subject to.
If the purpose of storage ceases to apply or if a storage period prescribed by the European Directive and Regulation Giver or another competent legislator expires, the personal data will be routinely blocked or deleted in accordance with the statutory provisions.
7 Rights of the data subject
a) Right to confirmation
Each data subject shall have the right granted by the European legislator to obtain from the controller the confirmation as to whether or not personal data concerning him or her are being processed. If a data subject wishes to avail himself of this right of confirmation, he or she may, at any time, contact any employee of the controller.
b) Right to information
Any person affected by the processing of personal data has the right, granted by the European legislator of directives and regulations, to obtain information free of charge at any time from the controller about the personal data stored about him/her and a copy of this information. Furthermore, the European legislator has granted the data subject access to the following information
the purposes of the processing
the categories of personal data being processed
the recipients or categories of recipients to whom the personal data have been or will be disclosed, in particular recipients in third countries or international organizations
where possible, the envisaged period for which the personal data will be stored, or, if not possible, the criteria used to determine that period
the existence of the right to request from the controller rectification or erasure of personal data or restriction of processing of personal data concerning the data subject or to object to such processing
the existence of the right to lodge a complaint with a supervisory authority
if the personal data are not collected from the data subject: All available information about the origin of the data
the existence of automated decision-making, including profiling, referred to in Article 22(1) and (4) of the GDPR and, at least in those cases, meaningful information about the logic involved, as well as the significance and envisaged consequences of such processing for the data subject
Furthermore, the data subject has a right to information as to whether personal data has been transferred to a third country or to an international organization. If this is the case, the data subject also has the right to obtain information about the appropriate safeguards in connection with the transfer.
If a data subject wishes to avail himself of this right of access, he or she may, at any time, contact any employee of the controller.
c) Right to rectification
Any person affected by the processing of personal data has the right granted by the European legislator of directives and regulations to demand the immediate correction of incorrect personal data concerning them. Taking into account the purposes of the processing, the data subject shall also have the right to have incomplete personal data completed, including by means of providing a supplementary statement.
If a data subject wishes to exercise this right to rectification, he or she may, at any time, contact any employee of the controller.
d) Right to erasure (right to be forgotten)
Any person affected by the processing of personal data has the right, granted by the European legislator, to obtain from the controller the erasure of personal data concerning him or her without undue delay where one of the following grounds applies and insofar as the processing is not necessary
The personal data have been collected or otherwise processed for such purposes for which they are no longer necessary.
The data subject withdraws consent on which the processing is based according to point (a) of Article 6(1) of the GDPR, or point (a) of Article 9(2) of the GDPR, and where there is no other legal ground for the processing.
The data subject objects to the processing pursuant to Article 21(1) GDPR and there are no overriding legitimate grounds for the processing, or the data subject objects to the processing pursuant to Article 21(2) GDPR.
The personal data has been processed unlawfully.
The personal data must be erased for compliance with a legal obligation in Union or Member State law to which the controller is subject.
The personal data have been collected in relation to the offer of information society services referred to in Article 8(1) GDPR.
If one of the aforementioned reasons applies, and a data subject wishes to request the erasure of personal data stored by the Cytoimmun Diagnostics GmbH, he or she may, at any time, contact any employee of the controller. An employee of Cytoimmun Diagnostics GmbH shall promptly ensure that the erasure request is complied with immediately.
If the personal data have been made public by Cytoimmun Diagnostics GmbH and our company, as the controller, is obliged pursuant to Art. 17 para. 1 GDPR, Cytoimmun Diagnostics GmbH shall take appropriate measures, including technical measures, taking into account the available technology and the implementation costs, to inform other data controllers who process the published personal data that the data subject has requested the deletion of all links to this personal data or of copies or replications of this personal data from these other data controllers, insofar as the processing is not necessary. An employees of the Cytoimmun Diagnostics GmbH will arrange the necessary measures in individual cases.
e) Right to restriction of processing
Any person affected by the processing of personal data has the right granted by the European legislator of directives and regulations to require the controller to restrict the processing if one of the following conditions is met:
The accuracy of the personal data is contested by the data subject, for a period enabling the controller to verify the accuracy of the personal data.
The processing is unlawful and the data subject opposes the erasure of the personal data and requests the restriction of their use instead.
The controller no longer needs the personal data for the purposes of the processing, but they are required by the data subject for the establishment, exercise or defense of legal claims.
The data subject has objected to processing pursuant to Article 21(1) GDPR pending the verification whether the legitimate grounds of the controller override those of the data subject.
If one of the aforementioned conditions is met, and a data subject wishes to request the restriction of the processing of personal data stored by the Cytoimmun Diagnostics GmbH, he or she may at any time contact any employee of the controller. The employee of Cytoimmun Diagnostics GmbH will arrange for the processing to be restricted.
f) Right to data portability
Each data subject shall have the right granted by the European legislator to receive the personal data concerning him or her, which he or she has provided to a controller, in a structured, commonly used and machine-readable format. He or she also has the right to transmit those data to another controller without hindrance from the controller to which the personal data have been provided, where the processing is based on consent pursuant to point (a) of Article 6(1) of the GDPR or point (a) of Article 9(2) of the GDPR or on a contract pursuant to point (b) of Article 6(1) of the GDPR and the processing is carried out by automated means, unless the processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller.
Furthermore, in exercising their right to data portability pursuant to Art. 20 (1) GDPR, the data subject has the right to have the personal data transmitted directly from one controller to another, where technically feasible and provided that this does not adversely affect the rights and freedoms of others.
In order to assert the right to data portability, the data subject may at any time contact any employee of the Cytoimmun Diagnostics GmbH.
g) Right to object
Each data subject shall have the right granted by the European legislator to object, on grounds relating to his or her particular situation, at any time, to processing of personal data concerning him or her, which is based on point (e) or (f) of Article 6(1) of the GDPR. This also applies to profiling based on these provisions.
The Cytoimmun Diagnostics GmbH shall no longer process the personal data in the event of the objection, unless we can demonstrate compelling legitimate grounds for the processing which override the interests, rights and freedoms of the data subject, or for the establishment, exercise or defense of legal claims.
If the Cytoimmun Diagnostics GmbH processes personal data for direct marketing purposes, the data subject shall have the right to object at any time to processing of personal data concerning him or her for such marketing. This also applies to profiling to the extent that it is related to such direct marketing. If the data subject objects to the Cytoimmun Diagnostics GmbH to the processing for direct marketing purposes, the Cytoimmun Diagnostics GmbH will no longer process the personal data for these purposes.
In addition, the data subject has the right, on grounds relating to his or her particular situation, to object to processing of personal data concerning him or her by the Cytoimmun Diagnostics GmbH for scientific or historical research purposes, or for statistical purposes pursuant to Article 89(1) of the GDPR, unless the processing is necessary for the performance of a task carried out for reasons of public interest.
In order to exercise the right to object, the data subject may contact any employee of the Cytoimmun Diagnostics GmbH. The data subject is also free, in the context of the use of information society services, and notwithstanding Directive 2002/58/EC, to exercise his or her right to object by automated means using technical specifications.
h) Automated decisions in individual cases including profiling
Each data subject shall have the right granted by the European legislator not to be subject to a decision based solely on automated processing, including profiling, which produces legal effects concerning him or her, or similarly significantly affects him or her, if the decision (1) is not necessary for entering into, or performance of, a contract between the data subject and the controller, or (2) is authorized by Union or Member State law to which the controller is subject and which also lays down suitable measures to safeguard the data subject's rights and freedoms and legitimate interests, or (3) is based on the data subject's explicit consent.
If the decision (1) is necessary for entering into, or the performance of, a contract between the data subject and a data controller, or (2) it is based on the data subject's explicit consent, the Cytoimmun Diagnostics GmbH shall implement suitable measures to safeguard the data subject's rights and freedoms and legitimate interests, at least the right to obtain human intervention on the part of the controller, to express his or her point of view and contest the decision.
If the data subject wishes to exercise the rights concerning automated individual decision-making, he or she may, at any time, contact any employee of the controller.
i) Right to withdraw consent under data protection law
Any person affected by the processing of personal data has the right granted by the European legislator of directives and regulations to withdraw consent to the processing of personal data at any time.
If the data subject wishes to exercise the right to withdraw the consent, he or she may, at any time, contact any employee of the controller.
8. legal basis of the processing
Art. 6 I lit. a GDPR serves our company as the legal basis for processing operations for which we obtain consent for a specific processing purpose. If the processing of personal data is necessary for the performance of a contract to which the data subject is party, as is the case, for example, when processing operations are necessary for the supply of goods or to provide any other service or consideration, the processing is based on Art. 6 I lit. b GDPR. The same applies to such processing operations that are necessary to carry out pre-contractual measures, for example in cases of inquiries about our products or services. If our company is subject to a legal obligation which requires the processing of personal data, such as for the fulfillment of tax obligations, the processing is based on Art. 6 I lit. c GDPR. In rare cases, the processing of personal data may become necessary in order to protect the vital interests of the data subject or another natural person. This would be the case, for example, if a visitor were injured in our company and their name, age, health insurance data or other vital information would have to be passed on to a doctor, hospital or other third party. The processing would then be based on Art. 6 I lit. d GDPR. Ultimately, processing operations could be based on Art. 6 I lit. f GDPR. Processing operations that are not covered by any of the aforementioned legal bases are based on this legal basis if the processing is necessary to safeguard a legitimate interest of our company or a third party, provided that the interests, fundamental rights and freedoms of the data subject do not prevail. We are permitted to carry out such processing operations in particular because they have been specifically mentioned by the European legislator. In this respect, it took the view that a legitimate interest could be assumed if the data subject is a customer of the controller (Recital 47 Sentence 2 GDPR).
9. legitimate interests in the processing pursued by the controller or a third party
Where the processing of personal data is based on Article 6 I lit. f GDPR our legitimate interest is to carry out our business in favor of the well-being of all our employees and our shareholders.
10. duration for which the personal data is stored
The criterion for the duration of the storage of personal data is the respective statutory retention period. After this period has expired, the corresponding data is routinely deleted, provided it is no longer required for the fulfillment or initiation of a contract.
11. legal or contractual provisions for the provision of personal data; necessity for the conclusion of the contract; obligation of the data subject to provide the personal data; possible consequences of non-provision
We inform you that the provision of personal data is partly required by law (e.g. tax regulations) or may also result from contractual provisions (e.g. information on the contractual partner). Sometimes it may be necessary for a contract to be concluded for a data subject to provide us with personal data that must subsequently be processed by us. For example, the data subject is obliged to provide us with personal data if our company concludes a contract with them. Failure to provide the personal data would mean that the contract with the data subject could not be concluded. Before personal data is provided by the data subject, the data subject must contact one of our employees. Our employee will inform the data subject on a case-by-case basis whether the provision of the personal data is required by law or contract or is necessary for the conclusion of the contract, whether there is an obligation to provide the personal data and what the consequences would be if the personal data were not provided.
12. existence of automated decision-making
As a responsible company, we do not use automated decision-making or profiling.
Developed by the Digital LegalTech specialists at Willing & Able, who also developed the system for data protection law and electronic working time recording. The texts of the data protection declaration generator were written by Prof. Dr. h.c. Heiko Jonny Maniero and lawyer Christian Solmecke.